Pancreatitis
UCI Health hepatobiliary specialists treat pancreatitis, a chronic or acute condition that inflames the pancreas, causing digestive enzymes to attack the very tissues that produce them.
At UCI Health, our pancreatic specialists can help restore your pancreas to health before your condition worsen.They work with you to find the best, most comprehensive treatment plan, including surgical and nonsurgical options.
Symptoms of pancreatitis
Pancreatitis is caused by inflammation of the pancreas, which causes digestive enzymes to attack the very tissues that produce them.
Pancreatitis can be either acute or chronic. Symptoms include:
- Gradual or sudden pain in the upper abdomen that may radiate through the back and is often worse after eating
- Tender or swollen abdomen
- Nausea and vomiting
- Rapid pulse
- Fever
- Weight loss
- Diarrhea
- Oily stools
If left untreated, severe pancreatitis can cause dehydration, low blood pressure and failure of other organs, including the kidneys, resulting in bleeding, shock and death.
Causes of pancreatitis
The most common causes of acute pancreatitis are:
- Gallstones—small crystals of hardened bile—that inflame the pancreas as they pass through the common bile duct
- Chronic alcohol abuse, which can inflame the pancreas within a few hours or days after consuming alcohol
- Abdominal trauma, medications, infections, tumors and genetic abnormalities of the pancreas
The most common causes of chronic pancreatitis are:
- Years of heavy alcohol use
- Hereditary disorders of the pancreas
- Cystic fibrosis—the most common inherited disorder leading to chronic pancreatitis
- Hypercalcemia—high levels of calcium in the blood
- Hyperlipidemia or hypertriglyceridemia—high levels of blood fats
- Some medications
- Some autoimmune conditions, including autoimmune pancreatitis
Both men and women experience pancreatitis. However, your risks for developing pancreatitis are higher if you are male.
If you are under age 30, you may go undiagnosed for pancreatitis for years. If you experience episodes of abdominal pain and diarrhea lasting several days, and which come and go over time, these can progress to chronic pancreatitis.
If you have two or more family members of different generations who have had pancreatitis, your risks of developing chronic pancreatitis are higher.
Autoimmune pancreatitis is caused by the body's immune system attacking the pancreas, and it can be mistaken for pancreatic cancer.
Diagnosis and testing for pancreatitis
Diagnosing acute pancreatitis can be difficult because of the location of the pancreas. In addition to a physical exam and blood tests, your physician may order one or more of the following tests:
- Abdominal ultrasound
- Computerized tomography (CT) scan
- Endoscopic ultrasound (EUS)
- Magnetic resonance cholangiopancreatography (MRCP)
Chronic pancreatitis is easily confused with acute pancreatitis. After a physical examination, your physician may order blood tests. In more advanced stages, your doctor may order blood, urine and stool tests to help diagnose chronic pancreatitis and monitor its progression.
Other tests include:
- X-rays
- Abdominal ultrasound
- CT, EUS and MRCP
Treatment for pancreatitis
Treatment for acute pancreatitis
If you are diagnosed with acute pancreatitis, our physicians will prescribe a treatment of intravenous (IV) fluids, antibiotics and pain medication. You will be required to stay at the hospital for a few days during this treatment.
In severe cases, you may need to be fed a special liquid delivered by a thin tube inserted through the nose, down the throat and into the stomach.
You will be advised to avoid fatty foods, alcoholic beverages and tobacco.
If gallstones are found to be the cause of your acute pancreatitis, surgical removal of the stones and the gallbladder may be recommended.
Acute pancreatitis sometimes causes kidney failure. If you experience kidney failure, dialysis or a kidney transplant may be required.
Treatment for chronic pancreatitis
If you are diagnosed with chronic pancreatitis, treatment may require hospitalization for pain management, intravenous hydration and nutritional support. Nasogastric feedings may be necessary for several weeks if you continue to lose weight.
When a normal diet is resumed, your physician may prescribe a regimen of synthetic pancreatic enzymes and a low-fat diet consumed in small, frequent meals.
Even if chronic pancreatitis is in its early stages, you should avoid alcoholic beverages and stop smoking.
Surgical intervention may be recommended in some cases. Procedures may include:
- Distal pancreatectomy (removal of the tail of the pancreas)
- Whipple procedure (removal of the head of the pancreas)
- Peustow procedure (drainage procedure)
- Beger or Frey procedure (resection and drainage procedure)
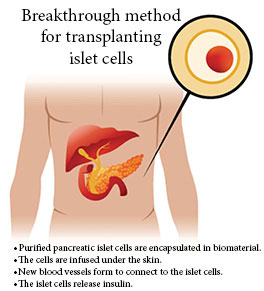
- Total pancreatectomy (removal of the entire pancreas) with auto islet cell transplant that was developed by our team
We are the only hospital in the region that performs extracorporeal shock wave lithotripsy, a non-invasive method that uses shock waves to break down stones in the kidney.
Chronic pancreatitis also may cause diabetes, triggering the need for insulin or other medication to maintain blood glucose levels.
Why Choose UCI Health for pancreatitis
Our UCI Health hepatobiliary specialists are part of a multidisciplinary team that comprises internists, medical oncologists and surgeons, as well as highly trained nurses and other clinical professionals.They will work with you to properly diagnose the form of your pancreatitis and its causes by conducting a comprehensive medical and genetic review, using the leading-edge technology, such as eyelid cell genetic processing conducted on site.
Following treatment, they will help you develop healthy choices that will keep your pancreas healthy and improve your quality of life, while our team of pain management specialists work with you to relieve postoperative pain.

Are you experiencing signs of pancreatitis?
Don’t delay treatment.
Call 888-717-4463 to schedule an appointment today, or

Find a digestive health clinical trial
Talk to your doctor to see if a digestive health clinical trial is right for you.
Featured Blog Posts

Delicious, diabetes-friendly meals

Diabetes patient helps others thrive
Diagnosed with type 1 diabetes at age 15, Jazmine Simon has aggressively managed her condition, determined to prevent it from disrupting her life. Now, she and her family underwrite a free UCI Health support group to help others cope with this deadly disease.