A new way to transplant insulin-producing islet cells
The 1921 discovery of insulin to treat type 1 diabetes hasn’t stopped scientists from trying to make life easier for the millions of people worldwide — including 1.6 million people in the United States — who are affected by the disorder.
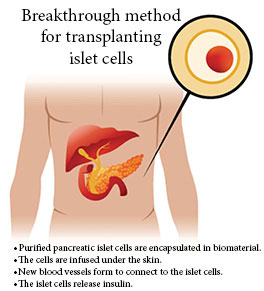
In recent years, transplanting pancreatic islet cells have offered an alternative to insulin injections. The insulin-producing islet cells restore the body's ability to regulate blood glucose levels, but the procedure poses serious challenges for patients, who have to take harsh immunosuppressant medications to prevent rejection.
Jonathan Lakey, PhD, and fellow UC Irvine researchers have developed a promising new method to transplant these cells to avoid triggering the body's immune system and eliminate the need for ongoing immunosuppressant therapy.
Encapsulating islet cells
In a recent paper published in the journal Communications Biology, Lakey, a UCI professor of surgery and biomedical engineering, and his team describe a biomaterial they developed to envelop the pancreatic islet cells so that when they are transplanted, the body doesn't view them as foreign invaders and mount an immune response.
It was Lakey who years ago co-developed a protocol proving the feasibility of pancreatic islet cell transplantation to treat type 1 diabetes at the University of Alberta.
Because treatment methods that use glucose pumps and continuous glucose monitors only prevent fluctuations in blood sugar on the surface level, the best approach is to find a way to replace the body's insulin-producing cells.
"But once you transplant tissue from one individual to another individual, you create an immune system response that tells the body to destroy the foreign cells,” Lakey says.
While immunosuppressant medications can halt the immune system’s response to the foreign cells, that approach is a lifelong commitment with significant risks. He and his team labored to find a better delivery system.
"Our concept is to use a biological material to contain and protect transplanted cells from the body,” he says
A new biomaterial
Lakey and Reza Mohammadi, who earned a doctorate in materials science and engineering at UCI last year while working in Lakey’s lab, helped develop a hybrid alginate — a material derived from seaweed.
This hybrid material releases exosomes — vesicles capable of transporting proteins and other substances between cells. The exosomes suppress the immune response, enabling the transplanted islet cells to function much longer.
In their study, Lakey and his colleagues showed that when implanted in diabetic mouse models, the encapsulated pancreatic islet cells did not evoke an adverse response.
The islet cells proceeded to successfully regulate blood glucose for more than 180 days without the need for insulin or anti-rejection therapies.
A stealth device
“The encapsulation is a stealth device, so the body doesn’t recognize it as foreign,” Lakey says. “The next step is to secure funding to take this technology into larger animals and, eventually, into humans.”
When he and his Canadian team first showed the feasibility of controlling insulin with islet cell transplantation, their findings generated considerable interest worldwide. It has taken more than 20 years to develop a promising way to circumvent the body's immune response.
“We’re very excited about the potential of this encapsulation technology," he says. "It’s early but very promising.”
The challenging nature of the work — supported by the Juvenile Diabetes Foundation, the Sue & Bill Gross Stem Cell Research Center and other groups — requires teamwork, which UCI offers in abundance. Colleagues in the schools of engineering, medicine, biological sciences, and pharmacy and pharmaceutical sciences have all contributed to this potential breakthrough, Lakey notes.
“UCI has exceptional facilities and a faculty that embraces collaboration.”




